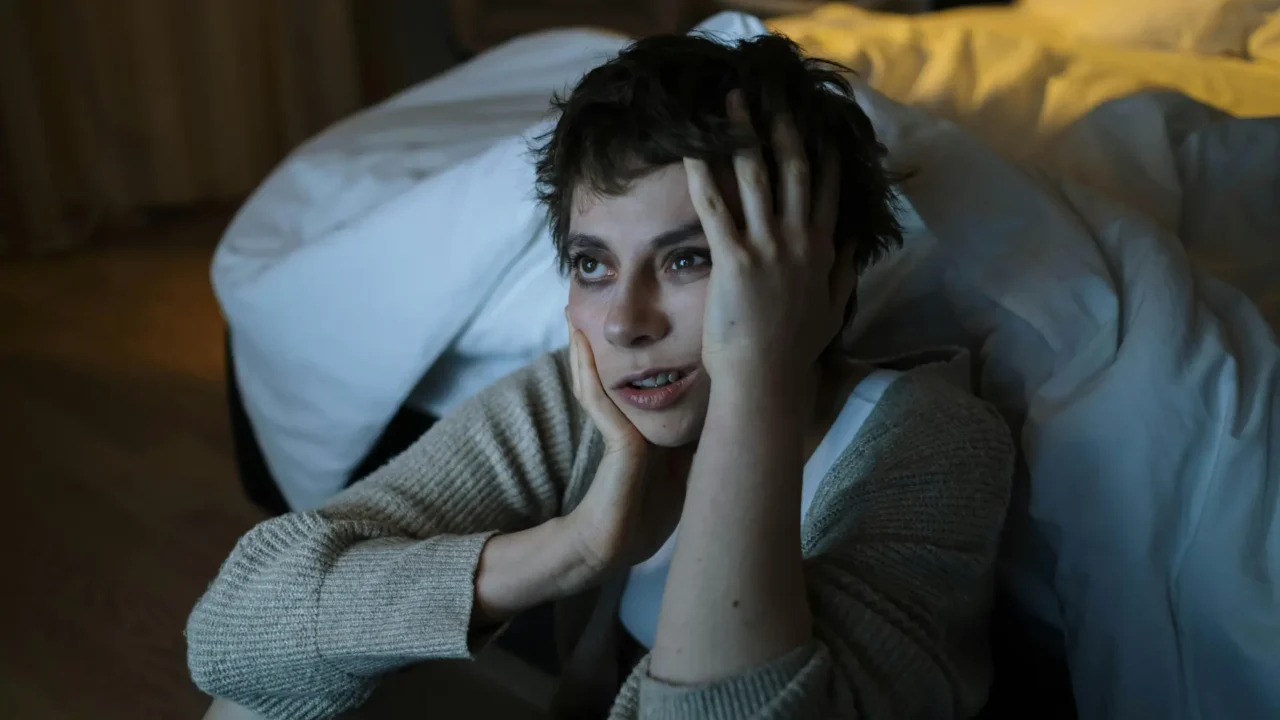
Sleep is one of the first things trauma disrupts. The connection between trauma and sleep is well documented, and survivors often describe lying awake for hours, jolting awake with nightmares, or feeling exhausted even after what looks like a full night of rest. These experiences are not “all in your head”; they are the body’s way of adapting to danger. The nervous system stays alert after trauma, releasing stress hormones that make it hard to fall asleep and stay asleep. According to the National Institute of Mental Health, heightened arousal and reactivity, such as difficulty falling or staying asleep and increased irritability, are core symptoms of post‑traumatic stress disorder (PTSD)[1]. Without restorative sleep, the body can’t repair tissues, consolidate memories, or regulate emotions, and trauma survivors may develop physical illnesses, mood disorders or weakened immunity.
How Trauma and Sleep Become Disrupted After Stressful Events
Trauma activates the body’s “fight–flight–freeze” response, which explains why trauma and sleep disturbances often develop together. Adrenaline surges and cortisol remains elevated to keep a person alert. When this state becomes chronic, it alters circadian rhythms and the hormones that control sleep. Nighttime becomes a time of vigilance rather than rest. Hypervigilance is often accompanied by muscle tension and a lower threshold for startle responses; this hyperarousal can persist for years[2]. Nightmares, vivid re‑enactments of traumatic events, are also common. They may cause people to avoid sleep altogether for fear of reliving the trauma. The Sleep Foundation notes that early after a traumatic event, nightmares are common and are considered part of the body’s normal stress response; however, when nightmares or insomnia persist, they may indicate PTSD[3].

The Health Consequences of Poor Sleep After Trauma
Ongoing sleep problems can exacerbate trauma symptoms. When trauma and sleep issues reinforce one another, emotional regulation becomes more difficult and physical health risks increase. Lack of REM sleep affects the brain’s ability to process emotions, making it harder to cope with daytime triggers. Sleep deprivation also increases inflammation and blood pressure, which are risk factors for chronic illness. Insomnia is associated with depression, anxiety, weight gain and weakened immune function. When a person is exhausted, they may rely on caffeine or alcohol to cope, which further disrupts sleep and can lead to addiction.
Evidence‑Based Strategies for Restful Sleep
Fortunately, there are effective strategies to restore healthy sleep patterns and address the root causes of trauma and sleep disruption. At Elnita Ottey & Associates, therapists integrate these evidence‑based approaches into treatment:
- Trauma‑focused psychotherapy and EMDR. Reprocessing traumatic memories through Eye Movement Desensitization and Reprocessing (EMDR) reduces nightmares and hyperarousal. EMDR allows the brain to store traumatic events in long‑term memory instead of continually re‑experiencing them. The National Institute of Mental Health notes that psychotherapy and exposure therapies can address PTSD symptoms and improve sleep[4].
- Image rehearsal therapy and lucid dreaming. For recurrent nightmares, clinicians may help clients rewrite the nightmare script while awake, then rehearse the new version before sleep. Lucid dreaming techniques train the dreamer to recognize they are dreaming and change the narrative, reducing distress[3].
- Sleep hygiene and relaxation. Good sleep hygiene includes maintaining a consistent bedtime, avoiding screens before bed, and creating a calm sleep environment. The Sleep Foundation recommends relaxing activities like gentle stretching or reading before bed and advises getting out of bed if you can’t sleep to break the association between bed and anxiety[3]. Deep breathing and progressive muscle relaxation signal the parasympathetic nervous system (“rest and digest”) to release tension.
- Medication when appropriate. In some cases, short‑term use of sleep medications may help reset sleep patterns. However, medication should always be used in combination with therapy and under medical supervision to avoid dependence[4].
Practical Tips for Building a Restful Routine
- Create a wind‑down ritual: dim lights, turn off screens an hour before bedtime, and engage in calming activities like journaling or listening to soothing music. Consider guided meditation apps that focus on trauma‑informed sleep.
- Set boundaries around news and social media: reading about violence or conflict before bed can increase anxiety. Give yourself permission to disconnect.
- Keep a dream journal: writing about nightmares can help you process them and work with your therapist on image rehearsal.
- Engage in daytime movement: gentle exercise or stretching reduces muscle tension and promotes deeper sleep.

When to Seek Professional Help
If sleep disturbances persist for more than a month after a traumatic event or if nightmares, panic attacks or flashbacks interfere with daily life, it may signal that trauma and sleep are becoming chronically dysregulated, and professional support is essential. At Elnita Ottey & Associates, therapists combine trauma‑informed approaches with sleep interventions to help clients reclaim their nights. Addressing underlying trauma is critical; sleeping pills alone do not resolve the root cause.
💡Trauma can significantly disrupt sleep, but healing insomnia and nightmares is possible. By understanding how trauma rewires the nervous system and employing strategies like EMDR, image rehearsal, and good sleep hygiene, survivors can gradually restore restful nights. Sleep is not a luxury; it is a cornerstone of mental and physical recovery. Reclaiming it is an act of self‑compassion and a vital step toward healing.
📍 In-person sessions available in Monroe, NC and the Charlotte Metro area.
🌐 Virtual sessions offered in NC, SC, TN, OK, CO, OR, and VT.
➡️ Learn more at www.elnitaottey.com or find a certified EMDR therapist at emdria.org